Relation of Cardiorenal Syndrome to Mitral and Tricuspid Regurgitation in Acute Decompensated Heart Failure
Frank F. Seghatol1*, Kimberly D. Martin2, Ayman Haj-Asaad1, Min Xie1, Sumanth D. Prabhu1
1Division of Cardiology, Department of Medicine, Washington University School of Medicine, USA
2Department of Medicine, Division of Cardiology and Department of Epidemiology, University of Alabama at Brimingham, Alabama, USA
*Corresponding author: Frank F. Seghatol, Division of Cardiology, Department of Medicine, Washington University School of Medicine, St. Louis, MO 63110, Missouri, USA; E-mail: s.frank@wustl.edu
Received: 29 September 2023; Revised: 13 October 2023; Accepted: 16 October 2023; Published: 18 October 2023
Copyright: © 2023 Seghatol FF. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Seghatol FF, Martin KD, Haj-Asaad A, Xie M, Prabhu SD. Cardiorenal Syndrome Complicating Treatment of Acute Decompensated Heart Failure: Relation to Mitral and Tricuspid Regurgitation. 21st Century Cardiol. 2023 October; 3(5):145
Citation:
Abstract
There is a complex interaction between the kidney and the heart. This interaction plays a major role both in normal physiology and in pathophysiology of heart or kidney failure. Renal dysfunction is one of the most important complications in patients with heart failure with reduced ejection fraction (HFrEF) and portends a poor prognosis.
Keywords:
Cardiorenal syndrom; Tricuspid regurgitation; Heart failure; Kidney
Description
There is a complex interaction between the kidney and the heart. This interaction plays a major role both in normal physiology and in pathophysiology of heart and kidney failure. Renal dysfunction is one of the most important complications in patients with heart failure with reduced ejection fraction (HFrEF) and portends a poor prognosis.
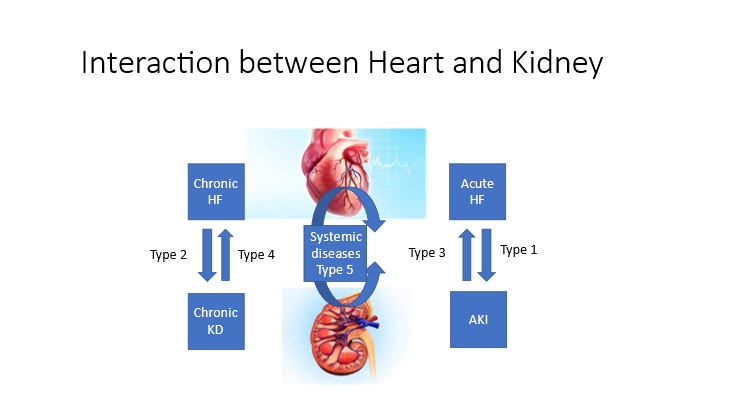
Figure 1: Classification and relationship between the heart and the kidney. In type 1 CRS acute HF like in cardiogenic shock leads to decrease cardiac output which leads to decrease renal blood perfusion. In type 2 CRS chronic reduction in blood flow to kidney associated with elevated filling pressure and congestion of splanchnic blood pool will lead to kidney failure through compression of renal veins. In type 3 CRS acute kidney injury will lead to fluid and salt retention which leads to volume overload and elevated filling pressures. In type 4 CRS chronically elevated volume overload leads to congestive heart failure. And type 5 CRS is when systemic diseases such as some forms of vasculitis and diabetes mellitus will affect both the heart and the kidney. (CRS: Cardiorenal Syndrome, HF: Heart Failure)
Cardiorenal syndromes are a group of linked disorders of the heart and kidneys. They are classified according to whether the problem is acute or chronic and whether the primary problem is in the heart (cardiorenal syndrome), the kidneys (renocardiac syndrome), or another organ (secondary cardiorenal syndrome). This classification is still evolving [1-2]. In Acute Decompensated Heart Failure National Registry (ADHERE) of 105000 patients admitted with acute decompensated heart failure (ADHF), 30% of patients had a previous history of renal insufficiency, 20% had creatinine > 2.0 mg/dl and 9% had creatinine >3.0 mg/dl [3].
Renal dysfunction is an independent risk factor for poor outcome and all-cause mortality in patients hospitalized with ADHF. Although worsening renal function was traditionally believed to result from decreasing cardiac output or diuretic-induced intravascular volume depletion, recent insights suggest that venous congestion has an important contributing role especially in the setting of an increasing serum creatinine during decongestive therapy [4].
It is also important to point out that the occurrence of rising serum creatinine has been more closely linked to inadequate fluid loss than drop in right atrial pressure.
However, if congestion persists and the ability for the kidney to mobilize fluid remains intact (e.g., diuretic-responsive), aggressive decongestive strategies may even overcome such counter-regulatory mechanisms [5]. Baseline GFR is a strong predictor of mortality, even more than left ventricular ejection fraction (LVEF) and NYHA functional class. Both elevated creatinine on admission and worsening creatinine during hospitalization predict prolonged hospitalization, re-hospitalization and death [6]. In all types of CRS, multiple pathophysiological processes are implicated in the initiation and progression of organ injury [7].
In our retrospective study we hypothesized that the presence of more than moderate mitral and/or tricuspid regurgitations (MR and/or TR) in patients with severe chronic heart failure with reduced ejection fraction (HFrEF) is associated with higher risk of developing cardiorenal syndrome (CRS). The reason for this hypothesis was that patients with moderate to severe or severe MR and TR are a subset of HFrEF who have both reduced cardiac output and elevated filling pressures. We recruited 80 consecutive patients who were hospitalized with acute decompensated heart failure due to HFrEF either from ischemic or non-ischemic cardiomyopathy.
All patients underwent comprehensive echocardiography within 24 H of admission. All measurements of cardiac chambers and Doppler evaluation were performed as recommended by the guidelines of the American Society of Echocardiography. The degree of mitral and tricuspid regurgitation (MR and TR) was evaluated semi quantitatively by visual assessment using the conventional views and quantitatively by measuring Vena Contracta (VC). Renal function as measured by BUN and Creatinine was measured on admission and on a daily basis during index hospitalization. An increase in Creatinine of > 0.3 mg/dl from baseline while receiving diuretic therapy was defined worsening renal function or cardio renal syndrome (CRS).
Our study shows that patients who develop CRS are those with baseline renal dysfunction and significant (moderately severe and severe) functional MR and/or TR. Comparison between the 2 groups shows that patients who develop CRS are those who have significant (at least moderate) MR and/or TR. Indeed, we found a statistically significant difference between the 2 groups in both the degree of visually estimated MR and TR (which is a semi-quantitative assessment of severity of regurgitation) and their vena contracta (vc) which is a quantitative measure of regurgitation.
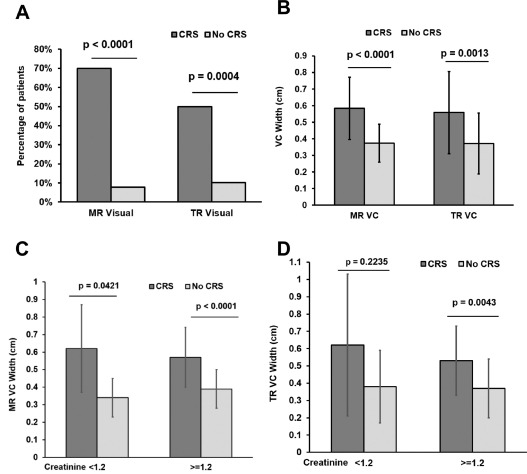
Figure 2: Severity of MR and TR is worse in patient with CRS. (A) Prevalence of moderate to severe or severe (3+ and 4+) MR and TR by visual assessment and by CRS status. (B) Mean MR and TR VC by CRS Status. (C) Mean MR VC by CRS Status stratified by baseline creatinine levels. (D) Mean TR VC by CRS Status stratified by baseline creatinine levels (CRS = dark gray bars, no CRS = light gray bars).
In addition to hemodynamic parameters, a constellation of biologic and molecular factors including endothelial injury, immunological imbalance, cell death, inflammatory cascades, oxidative stress, neutrophil migration, leukocyte trafficking, caspase-mediated apoptosis, extracellular vesicles, small noncoding RNAs, and epigenetics play pivotal roles in the development of CRS [7].
Our study shows the complex interaction between the heart and the kidney: patients with ADHF who develop CRS are those in whom the intrinsic renal function is more often initially abnormal compared to patients in whom renal function is intact. Moreover, our study shows that both decreased cardiac output and elevated filling pressures and elevated pressures in abdominal and splanchnic bed play an important role in the development of CRS.
Conclusion
Cardiorenal Syndrome has a complex pathophysiology. Chronic kidney disease and significant mitral and/or tricuspid regurgitation and probably RV systolic dysfunction are potential mechanisms of CRS. These factors should be considered when giving diuretic therapy in patients with ADHF and CRS.
Conflict of Interest Statement
Authors declare to have no conflict of interest relevant to this article.
References
1. Rangaswami J, Bhalla V, Blair JE, Chang TI, Costa S, Lentine KL, et al. Cardiorenal syndrome: classification, pathophysiology, diagnosis, and treatment strategies: a scientific statement from the American Heart Association. Circulation. 2019 Apr 16;139(16):e840-78. https://doi.org/10.1161/CIR.0000000000000664
2. Ronco C, Bellasi A, Di Lullo L. Cardiorenal syndrome: an overview. Adv Chronic Kidney Dis. 2018 Sep 1;25(5):382-90. https://doi.org/10.1053/j.ackd.2018.08.004
3. Adams Jr KF, Fonarow GC, Emerman CL, LeJemtel TH, Costanzo MR, Abraham WT, et al. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE). Am Heart J. 2005 Feb 1;149(2):209-16. https://doi.org/10.1016/j.ahj.2004.08.005
4. Orvalho JS, Cowgill LD. Cardiorenal syndrome: diagnosis and management. Vet Clin North Am Small Anim Pract. 2017 Sep 1;47(5):1083-102. https://doi.org/10.1016/j.cvsm.2017.05.004
5. Rubinstein J, Sanford D. Treatment of cardiorenal syndrome. Cardiol Clin. 2019 Aug 1;37(3):267-73. https://doi.org/10.1016/j.ccl.2019.04.002
6. Di Lullo L, Reeves PB, Bellasi A, Ronco C. Cardiorenal syndrome in acute kidney injury. Semin Nephrol. 2019 Jan 1; 39(1):31-40. https://doi.org/10.1016/j.semnephrol.2018.10.003
7. Ronco C, Di Lullo L. Cardiorenal syndrome. Heart Fail Clin. 2014 Apr 1;10(2):251-80. https://doi.org/10.1016/j.hfc.2013.12.003