Accurate Estimation of Right-Filling Pressure Using Handheld Ultrasound Score in Patients with Heart Failure
Authors: Wissam I Khalife1, Salman Salehin2, Izhan Hamza2, Muhammad Mushtaq2
Cardiology, University of Texas Medical Branch, Galveston, Texas, United States
Internal Medicine, University of Texas Medical Branch, Galveston, Texas, United States
*Correspondence to: Wissam Khalife, Division of Cardiovascular Disease, 301 University Blvd, Galveston, Texas 77555, USA; E-mail: Wikhalif@utmb.edu
Received: 26 November 2022; Accepted: 25 October 2022; Published: 29 October 2022
Citation: Khalife WI, Salehin S, Hamza I, Mushtaq M (2023) Accurate Estimation of Right-Filling Pressure Using Handheld Ultrasound Score in Patients with Heart Failure 21st Century Cardiol, Volume 3 (1): 126
Abstract
A crucial component of managing patients with heart failure involves an accurate and timely determination of intravascular volume status in the clinical setting. While physical exam can be helpful, it can also be challenging and often has a poor correlation with true volume status. The gold-standard test for accurate assessment of hemodynamic parameters, including right-sided filling pressures, is right heart catheterization [1]. However, this invasive modality is expensive, time consuming and prone to complications such as infection, thrombosis and iatrogenic procedure-related adverse events [2]. Alternatively, ultrasound has provided a quick, non-invasive, and fairly accurate way of determining volume status which allows clinicians to make accurate diagnoses and take appropriate therapeutic measures. Traditionally, right atrial (RA) pressure has been estimated by assessing inferior vena cava (IVC) size and its collapsibility with respiration using echocardiography or ultrasound. IVC size >21 mm and IVC respiratory non-collapsibility are associated with elevated RA pressures. Some studies have also found a correlation between internal jugular (IJ) vein respiratory variation and central venous pressure. However, the current body of evidence lacks a correlation of combined assessment of IVC, IJ dimensions, and respiratory collapsibility with RA pressures. Our institutional prospective study evaluated the correlation between RA pressure and the combined measurement of IVC/RIJ size and collapsibility with respiration. The study also aimed to investigate the statistical difference between assessing IVC alone and assessing IVC / RIJ together for evaluating RA pressure.
Keywords:
Introduction
A crucial component of managing patients with heart failure involves an accurate and timely determination of intravascular volume status in the clinical setting. While physical exam can be helpful, it can also be challenging and often has a poor correlation with true volume status. The gold-standard test for accurate assessment of hemodynamic parameters, including right-sided filling pressures, is right heart catheterization [1]. However, this invasive modality is expensive, time consuming and prone to complications such as infection, thrombosis and iatrogenic procedure-related adverse events [2]. Alternatively, ultrasound has provided a quick, non-invasive, and fairly accurate way of determining volume status which allows clinicians to make accurate diagnoses and take appropriate therapeutic measures. Traditionally, right atrial (RA) pressure has been estimated by assessing inferior vena cava (IVC) size and its collapsibility with respiration using echocardiography or ultrasound. IVC size >21 mm and IVC respiratory non-collapsibility are associated with elevated RA pressures. Some studies have also found a correlation between internal jugular (IJ) vein respiratory variation and central venous pressure. However, the current body of evidence lacks a correlation of combined assessment of IVC, IJ dimensions, and respiratory collapsibility with RA pressures. Our institutional prospective study evaluated the correlation between RA pressure and the combined measurement of IVC/RIJ size and collapsibility with respiration. The study also aimed to investigate the statistical difference between assessing IVC alone and assessing IVC / RIJ together for evaluating RA pressure.
Discussion
Presently the ASE (American Society of Echocardiography) guidelines consider maximum IVC diameter and the degree of inspiratory collapse of the distal tract of the IVC as surrogate markers of RA pressure. A combination of maximum IVC diameter > 21 mm and collapsibility with respiration <50% suggests a high right atrial pressure (RAP) of ~15 mmHg. On the other hand, IVC diameter ≤ 21 mm coupled with collapsibility ≥ 50% indicates a normal RAP of 0-5 mmHg. In cases where a maximum IVC diameter ≤ 21 mm is coupled with a collapsibility < 50%, or where a maximum IVC diameter > 21 mm is coupled with a collapsibility ≥ 50%, the RAP is estimated to be between 5-10 mm Hg, although the interpretation is less clear [3]. Assessment of volume status based exclusively on IVC parameters runs the risk of a high margin of error given that the IVC becomes inelastic and flared at the RA junction in patients with prolonged heart failure. Additionally, the sonographic visualization of the IVC can be limited due to abdominal distension, bowel gas overlying the IVC, tissue edema, ascites, complex abdominal wounds, and morbid obesity. Therefore, lies the value of non-abdominal venous assessment of right atrial pressure.
The addition of the right internal jugular (RIJ) vein collapsibility as part of a 3-point score circumvents this problem and improves specificity. We postulated that this additional third point would further improve the utility of non-invasive ultrasound in RA pressure estimation. Previous studies have already established the utility of IJV in estimation of RA pressure despite the IVC being regarded as the better surrogate. Our institutional prospective study evaluated the correlation between RA pressure and the combined measurement of IVC/RIJ size and collapsibility. The study also aimed to investigate the statistical difference between assessing IVC alone and assessing IVC / RIJ together for evaluating RA pressure.
Receiver operating characteristic curves (Figure 1) were used to compare the diagnostic performance of the 3- point scoring system (IVC and RIJ end-inspiratory non-collapsibility and IVC size ≥ 21 mm) versus the 2-point scoring system (IVC end-inspiratory non- collapsibility and IVC size ≥ 21 mm) in estimation of elevated RA pressures. The addition of RIJ respiratory collapsibility led to increased accuracy in RA pressure estimation, as evidenced by an increase in area under the curve (AUC) from 0.75 for the 3-point score to 0.84 for the 2-point score with a significant P value (AUC 0.75 [0.67-0.83] vs 0.84 [0.77-0.92]; P=0.003). Furthermore, the 3-point score has a relatively higher specificity of 97% despite having a lower sensitivity (Table 1).
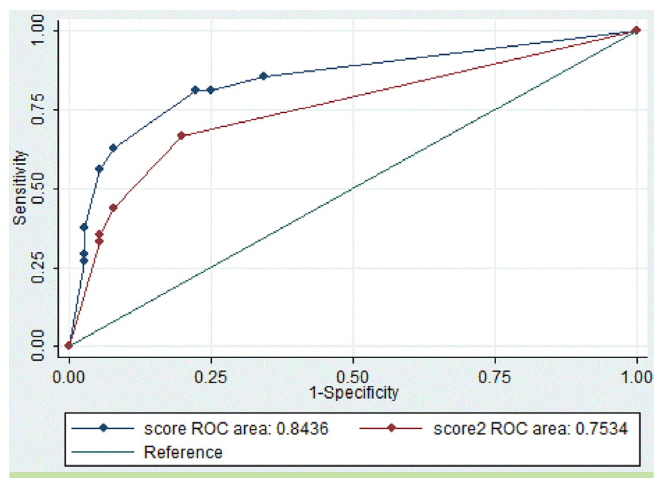
Figure 1: Comparison of 3-point score (using RIJ respiratory non-collapsibility, IVC dimension ≥21 mm, IVC respiratory non-collapsibility) AUC with 2-point score (IVC dimension ≥21 mm, IVC respiratory non-collapsibility) AUC.
Score: Refers to the 3-point score; score 2: refers to the -point score. AUC = area under the curve; IVC = inferior vena cava; RIJ = right internal jugular vein.
Table 1: IVC/IJ score at different cut point with 95% confidence interval.
|
IVC/IJ score |
Sensitivity |
Specificity |
PPV |
NPV |
|
0 |
100% |
0% |
22% (15-29) |
- |
|
1 |
85% (79-91) |
66% (58-74) |
42% (34-50) |
95% (91-99) |
|
2 |
63% (55-71) |
92% (87-97) |
69% (61-77) |
90% (85-95) |
|
3 |
29% (21-37) |
97% (94-100) |
71% (63-79) |
83% (76-90) |
|
IJ = internal jugular; IVC = inferior vena cava; NPV = negative predictive value; PPV = positive predictive value |
||||
The score also outperformed physical examination (lower extremity edema, rales and jugular venous distension) in predicting volume status (RA pressure). 58% (24/41) of patients were correctly diagnosed to have elevated RA pressure ≥ 10 whereas 83% (30/36) patients with score ≥ 2 were appropriately identified to have RA pressure ≥ 10; in each case, right cardiac catheterization was utilized to validate the RA pressure. Similarly, Brennan et al. demonstrated that the assessment of the size & collapsibility of IVC can predict increased RA pressure more frequently and accurately than with physical assessment of the jugular venous distension.
This improvement further enhances the utility of handheld ultrasound in ruling in a diagnosis of heart failure and will help guide critical decisions in therapy. For instance, it will enable physicians to reliably determine the degree of residual hemodynamic congestion. Despite their apparent euvolemia, many heart failure patients may still be hypervolemic at the time of hospital discharge, as evidenced by the high readmission rate for those patients. The rate of 30-day HF rehospitalization in the claims databases of the USA and in worldwide randomized clinical trials is 20–25%6–10 and 5–10%,11,12 respectively. Several studies have shown that adjusting diuretic dosage based solely on clinical criteria carries a substantial risk of therapeutic errors, either potential risk of short-term recurrence of heart failure exacerbation or the risks associated with over diuresis [4]. Apart from the morbidity and mortality associated with frequent readmissions, there is also a heavy financial strain on the already stretched US health care system.
Despite the effectiveness of the handheld ultrasound in the assessment of volume status, the 2-point or the 3-point system is yet to become standard of care. This may be due to paucity of outcome data studies showing reduction in heart failure readmissions by ultrasound-based approach as well as frequent use of echocardiography and right heart catheterization in the inpatient setting.
Patel et al tried to incorporate 3D echo imaging in addition to IVC diameter, however despite achieving similar accuracy and specificity gains and better sensitivity gains. The updated ASE guidelines did not include 3D echocardiography as a tool for RA pressure estimation, possibly due to the additional time, complexity and cost associated with 3D echocardiography. Our 3-point method has advantages over the aforementioned method. It utilizes portable handheld ultrasounds, thus more likely to have broader clinical adaptation at limited additional cost. Compared to the other peripheral venous estimation (such as subclavian vein) for estimation of RA pressure, the RIJ has the advantage of being more superficial and thus less likely to be obscured by body cavities or tissue. However, the shallow course of the RIJ increases susceptibility to external compression by the sonographer, which can affect its respiratory collapsibility. Additionally, the RIJ is more prone to variation with body position than the IVC. In our study all patients were 0 degrees spine angle to emulate cardiac catheterization settings and IJ compressibility was performed by expert sonographers, unfamiliar finding in most POC (Point of Care) settings. Lastly, all sonographic assessments are prone to intra- and inter- observer variability making their utility user dependent. All these factors may limit the use of the 3-point system as POC test by providers. However, formal sonography training can overcome all these limiting factors.
Conclusion
The addition of RIJ respiratory collapsibility to assessment of IVC dimension and collapsibility has enhanced the diagnostic utility of handheld ultrasound in RA pressure estimation. The ultrasound-based approach provides a powerful tool to guide the management of heart failure patients. Long-term outcome data studies are vital to divulge its true benefit, and ultimately persuade its incorporation into clinical practice.
